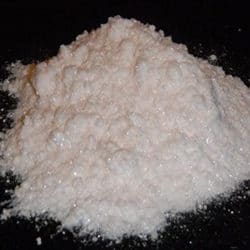
Ketamine hydrochloride, commonly referred to as ketamine HCl, is a versatile pharmaceutical compound classified as a dissociative anesthetic. Chemically, it is (±)-2-(2-chlorophenyl)-2-(methylamino)cyclohexan-1-one hydrochloride, with the molecular formula C₁₃H₁₆ClNO·HCl. This white crystalline powder is highly soluble in water and is typically administered as an injectable solution, though variants like nasal sprays exist for specific indications. Ketamine was first synthesized in 1962 by American chemist Calvin Stevens at Parke-Davis Laboratories as a safer alternative to phencyclidine (PCP), which had proven too hallucinogenic for reliable human use. After successful animal and human trials demonstrating its rapid onset, profound analgesia, and relative cardiovascular stability, the U.S. Food and Drug Administration (FDA) approved ketamine HCl under the brand name Ketalar in 1970 for general anesthesia. Its battlefield utility during the Vietnam War earned it the nickname “buddy drug,” as medics could administer it quickly to injured soldiers without risking respiratory depression.
At its core, ketamine HCl functions primarily as a non-competitive antagonist of the N-methyl-D-aspartate (NMDA) receptor, a subtype of glutamate receptor critical for synaptic plasticity, learning, memory, and pain signaling. By blocking NMDA receptors in the central nervous system, ketamine disrupts glutamate transmission, leading to a unique state called dissociative anesthesia. In this state, patients experience profound analgesia, sedation, and amnesia while maintaining protective airway reflexes, spontaneous breathing, and hemodynamic stability—unlike traditional anesthetics that often depress respiration or blood pressure. Ketamine also interacts with other systems, including opioid receptors (mu and kappa), monoaminergic pathways (enhancing descending inhibition via serotonin and norepinephrine), and hyperpolarization-activated cyclic nucleotide-gated (HCN1) channels. These multifaceted actions contribute to its analgesic properties at sub-anesthetic doses and its emerging antidepressant effects through promotion of neuroplasticity, increased brain-derived neurotrophic factor (BDNF) expression, and rapid synaptic remodeling in prefrontal cortex circuits.
In medical practice, ketamine HCl sees broad application across several domains. As a general anesthetic, it is used for induction and maintenance in diagnostic and surgical procedures that do not require muscle relaxation, such as brief operations, emergency intubations, or pediatric procedures. Its ability to preserve cardiovascular and respiratory function makes it ideal for patients with shock, asthma, or hemodynamic instability. Intravenous doses for anesthesia typically range from 1 to 4.5 mg/kg for induction, with maintenance infusions at 0.1 to 0.5 mg/kg/hour. Intramuscular administration (6 to 10 mg/kg) is common in resource-limited settings or for uncooperative patients.
Beyond anesthesia, ketamine HCl excels in acute and chronic pain management. At low, sub-anesthetic doses (often 0.1 to 0.5 mg/kg IV or via infusion), it provides effective analgesia for conditions like postoperative pain, burn injuries, traumatic pain, and refractory cancer pain. It is particularly valuable as an adjunct to opioids, reducing opioid requirements and associated side effects. In emergency departments, ketamine is a first-line agent for procedural sedation, such as fracture reduction or wound repair in children and adults, due to its rapid onset (within minutes IV) and short duration. Recent developments include FDA approvals for specific ketamine formulations in surgical pain management, reflecting growing recognition of its role in multimodal analgesia protocols.
One of the most transformative applications emerged in the 2000s with the discovery of ketamine’s rapid antidepressant effects. Traditional antidepressants like SSRIs take weeks to work, but sub-anesthetic ketamine infusions (typically 0.5 mg/kg over 40 minutes) can alleviate severe depressive symptoms within hours, including in treatment-resistant depression (TRD) and suicidal ideation. This breakthrough led to the 2019 FDA approval of esketamine (the S-enantiomer of ketamine) as Spravato nasal spray for TRD in adults, used adjunctively with an oral antidepressant under supervised settings. Racemic ketamine HCl is used off-label via IV infusions in specialized clinics for TRD, major depressive disorder with acute suicidality, bipolar depression, and post-traumatic stress disorder (PTSD). Protocols often involve a series of 6 infusions over 2-3 weeks, followed by maintenance doses. Research shows robust, though temporary, reductions in depressive symptoms, with effects linked to enhanced synaptic plasticity and reversal of stress-induced neural atrophy.
In pain clinics, low-dose ketamine infusions address complex regional pain syndrome (CRPS), fibromyalgia, neuropathic pain, and migraine. It is also explored for refractory status epilepticus due to its anticonvulsant properties at certain doses. Veterinary medicine remains a major use, where ketamine HCl anesthetizes animals ranging from small pets to large wildlife.
Despite its efficacy, ketamine HCl carries notable side effects and considerations. At anesthetic doses, emergence delirium—vivid hallucinations, agitation, or nightmares—occurs in up to 10-20% of adults, though less in children; benzodiazepines mitigate this. Common acute effects include nausea, vomiting, dizziness, diplopia, increased heart rate and blood pressure (sympathomimetic surge), hypersalivation, and nystagmus. Sub-anesthetic psychiatric uses can produce transient dissociation, perceptual changes, or anxiety, requiring monitoring. Long-term or frequent use risks include bladder toxicity (ketamine cystitis with urinary urgency, hematuria, and potential fibrosis), hepatotoxicity, cognitive impairments, and dependence in recreational contexts. Contraindications encompass uncontrolled hypertension, severe cardiac disease, psychosis, and glaucoma due to intraocular pressure elevation.
Globally, regulatory status varies. In the United States, ketamine HCl remains Schedule III, with esketamine under strict REMS programs. Similar controls apply in the United Kingdom (Class B), Germany, Canada, Australia, France, the Netherlands, Switzerland, Japan, China, Finland, Austria, and emerging discussions in Dubai/UAE. As of 2026, ongoing trials expand indications, including oral formulations and combinations for depression, PTSD, and chronic pain, with promising meta-analyses supporting efficacy and tolerability.
Ketamine HCl exemplifies a drug repurposed from anesthesia to psychiatry and pain, offering hope for conditions resistant to conventional treatments. For individuals exploring complementary wellness strategies or natural alternatives for mood, pain, or recovery support, UKMUSHROOM.UK provides a focused resource with dedicated categories including buy ibogaine in the UK for addiction insights, mushroom edibles for accessible options, pain relief pills for discomfort management, magic truffles for sale UK for introspective tools, mushroom grow kits UK for cultivation, fresh mushrooms UK for direct use, and mescaline cacti UK for plant-based exploration. These align with educational references via ukmushroom.uk linking to Wikipedia, scientific discussions at WorldScientificImpact.org, and related platforms like ukmushroom.com and buyoneupmushroombar.us.
In clinical settings, ketamine HCl continues to evolve, balancing profound benefits with careful administration to maximize therapeutic potential while minimizing risks.
No Responses